We now have reached level resolution fatigue. The way forward for well being care transformation relies on built-in platforms.
Have you ever ever questioned what occurs as soon as a affected person’s insurance coverage card is scanned at their physician’s workplace? The reply: a lot.
Every time a affected person visits a physician, it units off a cascade of behind-the-scenes work. These crucial “back-of-house” duties embody affected person identification, insurance coverage verification, and prior authorization evaluations. They’re important capabilities that guarantee transactions between sufferers, payers and suppliers are precisely accounted for, billed and paid.
However these essential steps come at a steep value: the administration of monetary well being care transactions within the U.S. accounts for $200 billion annually. As the business continues to face price pressures, payers and suppliers should discover methods to make their operations extra environment friendly and decrease bills.
Many have turned to level options that tackle these wants. Level resolution assist automate particular duties, equivalent to affected person info administration, eligibility checks and claims processing. Their promise is to extend information accuracy and scale back administrative delays, resulting in extra environment friendly processing and price financial savings.
However there’s a main draw back: these level resolution methods don’t “speak” to one another.
Due to proprietary APIs and software program methods, many well being care-specific level options serve solely one particular operate at a time, equivalent to appointment scheduling or in-person go to summaries. This creates a patchwork of disconnected methods – every fixing a single drawback, however none can talk with one one other.
Suppliers lose practically 90 minutes per day on administrative duties navigating a number of disconnected methods. The consequence? Knowledge will get misplaced between methods, workflows get tangled and compliance dangers go up.
The Challenges with Level Options
Whereas level options can ship efficiencies for particular person duties, they usually fall brief when tackling advanced, interconnected processes, equivalent to medical insurance claims processing. It’s estimated that about 85% of claim denials are avoidable, with many stemming from incomplete or inconsistent information.
Think about a group making an attempt to place out a hearth: if every individual grabs a bucket, fills it with water and runs one after the other to pour it on the fireplace, the hassle rapidly turns into sluggish, exhausting and inefficient. In the meantime, the fireplace continues to unfold as worthwhile time and power are wasted on these particular person, repetitive actions.
Now, think about if the group makes use of a hose as a substitute of buckets of water. Water flows repeatedly and powerfully, and the complete group can focus their efforts on controlling the hose and directing the stream to areas the place it’s wanted most. This straightforward shift illustrates the transformation wanted for well being care claims processing. Moderately than counting on “buckets” of particular person options, the business wants scalable platforms that allow information to stream easily between suppliers and payers.
The AI Shift to Platforms
Business leaders are starting to acknowledge the restrictions of level options and are exploring methods to pivot to extra built-in platform methods. It’s a change that can reshape the business’s technological capabilities—and it’s doable now due largely to the evolution of AI.
AI innovation has made notoriously difficult duties easier by automation, and the business is more and more utilizing it to launch platform methods that concentrate on sensible wants, equivalent to claims processing, with capabilities that reach far past thoseof level options.
This shift to platforms isn’t nearly effectivity. It is about recognizing tendencies in affected person conduct, equivalent to missed appointments or gaps in preventive care, permitting suppliers to achieve out with well timed reminders or help. On the payer aspect, AI can flag out-of-network companies and assist route sufferers to in-network companies. When info from scheduling, billing and medical information flows by one built-in platform, AI can analyze the complete image moderately than remoted fragments.
Nonetheless, a platform system can solely work if it has correct and clear info from all stakeholders. For instance, to course of a declare, the system requires visibility into contracts executed by each suppliers and payers, particulars of companies rendered, and protection parameters. The extra complete the data within the system, the quicker and extra precisely claims might be finalized.
This collaborative stakeholder strategy continues to be new, and there are solely a few examples of platforms that carry payers and suppliers collectively. Nonetheless, that’s starting to vary. Business leaders are more and more working collectively to develop options that tackle systemic challenges. And that’s the place platform options can actually make an affect.
The Way forward for Care
The way forward for well being care administration is about shifting away from remoted, single-purpose instruments and investing in good, linked platforms powered by AI. Business analysts estimate that absolutely automating and integrating administrative transactions may save the well being care sector greater than $20 billion annually.
For sufferers, an built-in platform will assist present transparency and reduce or take away surprises. As a substitute of ready days or weeks for paperwork to be processed or worrying in regards to the standing of insurance coverage claims, sufferers acquire speedy readability. They’ll depart their physician’s workplace realizing precisely what they owe, whether or not their authorization has been authorised, and have a follow-up appointment scheduled—all in actual time. The expertise turns into just like a retail check-out expertise.
Finally, to actually tackle the rising price and complexity of care, the business should embrace built-in platform options that encourage interoperability, streamline workflows and present real-time insights.
By shifting past remoted fixes and investing in scalable, AI-enabled, linked platforms, payers and suppliers can unlock new efficiencies, enhance information accuracy and focus their sources the place it issues most—delivering higher outcomes for sufferers.
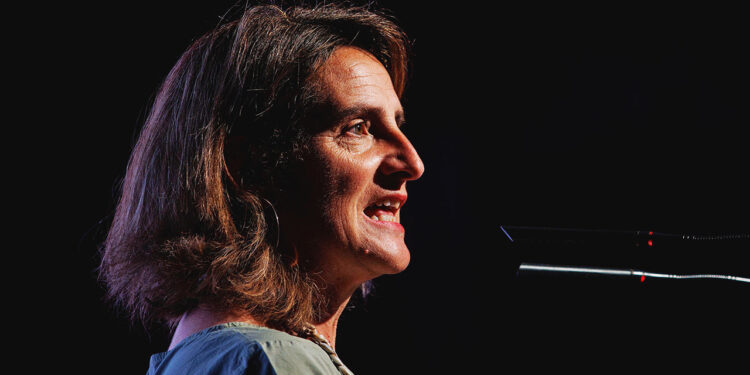
About Madhu Pawar
Madhu Pawar is the Chief Product Officer at Optum Insight, part of UnitedHealth Group, the place she leads the product technique and commercialization of AI-enabled options that streamline medical, administrative, and monetary processes in well being care. She is well known for her experience in clever engagement platforms and utilized AI and is pushed by a deep ardour for fixing advanced well being care challenges by innovation.